Medicaid is a federal and state-funded health insurance program that provides full coverage for some vulnerable low-income North Carolinians. It improves access to healthcare and health outcomes for North Carolinians by increasing access to primary care providers, regular checkups, preventative care, and care for chronic conditions.
There are many different types or categories of Medicaid, each with its own income limits compared to the federal poverty line (FPL). Medicaid expansion is the newly implemented program in the state of North Carolina, covering adults aged 19-64 who meet the income requirements. This expands coverage to college students, working parents, childless adults, and more.
Have questions or think you may be eligible? Make a free appointment with a Health Insurance Navigator at Charlotte Center for Legal Advocacy Call 980-256-3782 or visit the website ncnavigator.org to schedule your free phone appointment today!
- On March 27, 2023, Governor Cooper signed the Medicaid Expansion into law.
- NC is the 41st state to expand Medicaid (Including the District of Columbia)
- As March 2025, more than 630,000 people have enrolled in Medicaid Expansion
Who will be able to get health coverage through NC Medicaid?
Most people can get health care coverage through NC Medicaid if they meet the criteria below. If you were eligible before, you still are. Eligibility criteria:
- You live in North Carolina
- Age 19 through 64
- You are a citizen (some non-U.S. citizens can get health coverage through NC Medicaid)
- If your household income fits within the following chart:
Click here for a Medicaid PDF with more information.
What should I do?
To apply contact your local DSS office or schedule a free appointment with a Health Insurance Navigator by calling 980-256-3782 or visiting www.ncnavigator.org.
- Contact your local DSS office to make sure they have your current mailing address, phone number, email, and other contact information.
- Local DSS Offices:
- Mecklenburg County
- 704-336-3000
- Wallace H. Kuralt Centre, 301 Billingsley Road, Charlotte, NC 28211
- Community Resource Center, 3205 Freedom Drive, Charlotte, NC 28208
- Union County
- 704-296-4300
- 2330 Concord Avenue Monroe, NC 28110
- Cabarrus County
- 704-920-1400
- 1303 S. Cannon Blvd. Kannapolis, NC 28083
- Mecklenburg County
- Local DSS Offices:
- Watch for mail, texts, or phone calls from DSS and respond promptly.
- Create an enhanced E-Pass account (https://epass.nc.gov):
- View your benefits,
- Upload documents supporting any changes, like income or household size,
- Update your information online
If you are denied and think it is wrong, we may be able to help. Call 704-376-1600 (select public benefits option) or make an appointment online.
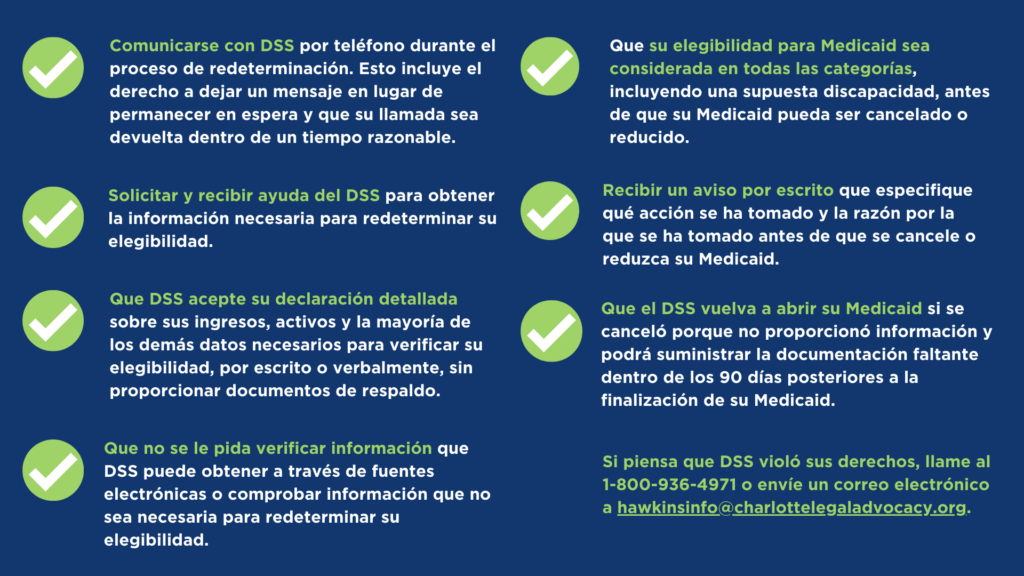
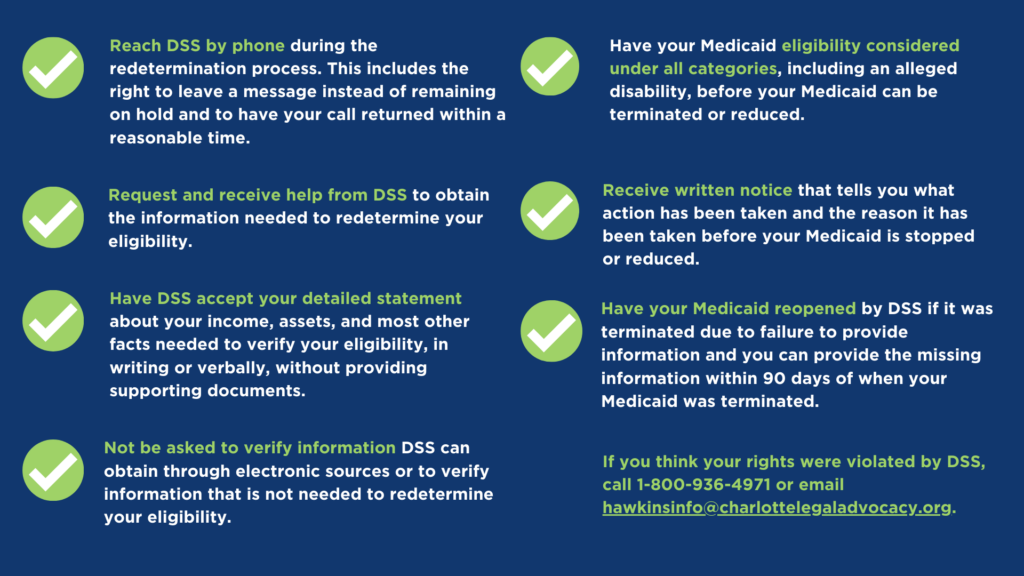
You have the right to:
You have the right to appeal.
If you believe there has been an error, you can appeal that decision. You have 60 days (about 2 months) from the date of the notice to ask for an appeal. If you do so within 10 business days, you can request that your Medicaid be continued while the appeal is reviewed. Call 704-376-1600 and press 2 (public benefits) for more information or make an appointment online.
Special Enrollment Periods (SEP) are available for Medicare and Marketplace coverage.
Individuals who are no longer eligible for Medicaid may be eligible to enroll in Medicare or Marketplace coverage with a special enrollment period.
- Health Insurance Navigators can provide more information and offer free help enrolling in the Marketplace.
- 980-256-3782
- charlottelegaladvocacy.org/getcovered or ncnavigator.net
- SHIIP counselors offer free and unbiased information regarding Medicare health care products and eligibility
- 1-855-408-1212
Free legal assistance may be available.
If you think your Medicaid was wrongfully reduced or terminated, call 704-376-1600 and press 2 (public benefits) or make an appointment online.
For more helpful resources, visit NCMedHelp.org.