North Carolina Medicaid Managed Care- What is it and how does it affect my Medicaid coverage?
North Carolina has undergone a change in how Medicaid benefits are set-up. This change, called the Medicaid Transformation, has caused many Medicaid-eligible individuals to be switched from the traditional Medicaid Direct, managed by the state of North Carolina, to new health plans that are managed by private companies instead. This change took place officially July 1, 2021, but many people are still left with questions about how the changes affect them. Answers to some common questions are below, as well as guidance on where to go for help.
Am I still eligible for Medicaid?
While the way benefits and services are managed has changed, Medicaid eligibility criteria are the same under the new Managed Care system. If you want to report changes to your situation (address, income, etc.) or if you want to apply for Medicaid, you will still need to contact your local Department of Social Services (DSS) office.
Am I enrolled in one of the new Medicaid health plans?
You may have selected a Prepaid Health Plan (plan or PHP) to manage your health care, either during the enrollment period or when you applied for Medicaid. If you didn’t select a plan, you may have been automatically enrolled in one. If you were automatically enrolled in a health plan, you should have received a packet from your health plan with a new Medicaid card. If you are not sure which plan you are in, or if you have not received a card form you plan, you can call the Enrollment Broker at 833-870-5500 (TTY: 833-870-5588).
Where can I learn about the health plan benefits?
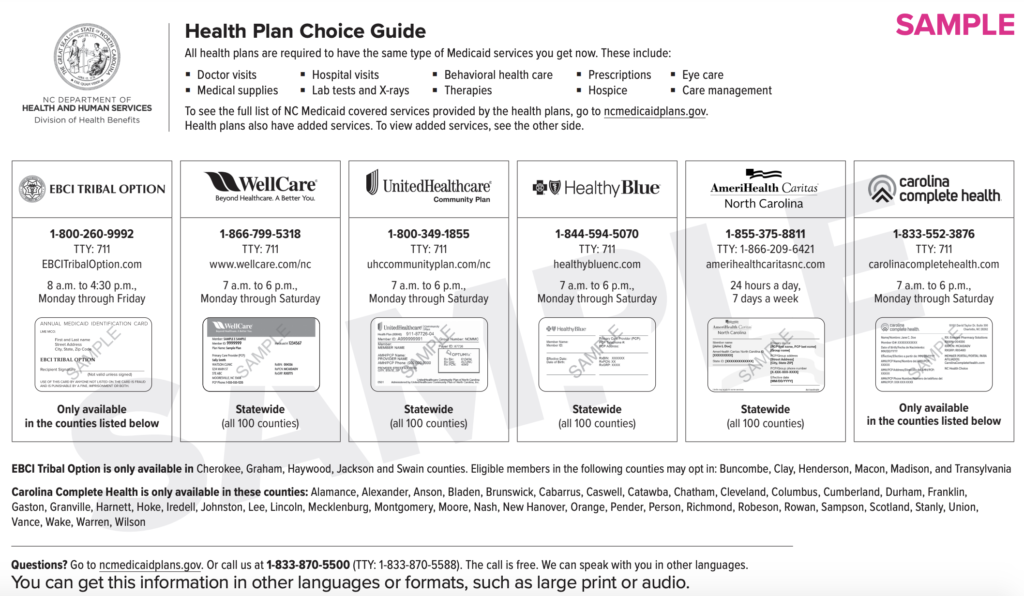
You can learn about the plans below and online.
What if I want to switch to a different Medicaid plan?
You have 90 days after coverage under your new Managed Care health plan begins to change to a different health plan for any reason. For beneficiaries whose coverage began July 1, this choice period ended September 30. However, you can still switch to a different health plan after this choice period if you have a special reason to do so, If you want to request to switch to a different plan, call the Enrollment Broker at 833-870-5500 (TTY: 833-870-5588) or submit the Health Plan Change Request form, found here.
If you have any problems or unanswered questions, the NC Medicaid Ombudsman is a resource to answer questions and help resolve issues about the move to Medicaid Managed Care. You can reach them at 877-201-3750 from 8 a.m. to 5 p.m. Monday through Friday, except State holidays, or you can visit their website at ncmedicaidombudsman.org.
How do I use my new Medicaid card?
Providers should NOT require you to show your physical Medicaid ID card in order to see you at your appointment.
What if some of my doctors don’t accept the new Medicaid plan?
Each health plan has a group of providers called a network, and you’ll usually have to go to providers in your plan’s network. We recommend you confirm with your medical providers that they are in network with your health plan, and call your plan if you have any questions about what services you can receive and what providers you can see. If your provider has not contracted with your health plank, so they are not in your plan’s network, you may have to see another provider who does accept your plan. However, depending on your situation, you may be able to switch to a different plan to continue seeing your provider. You can contact the Enrollment Broker at 833-870-5500 (TTY: 833-870-5588) or submit the Health Plan Change Request Form to make this request.
What about my dental and vision coverage?
Some services are not covered through your new health plan and will continue to be covered through NC Medicaid Direct (traditional Medicaid). These services are known as “carved out” services, and include dental services and the fabrication of eyeglasses (however other vision services are managed by your health plan). For these carved out services, you can see any provider who accepts Medicaid, rather than only providers in your health plan’s network.
How do I schedule transportation to my appointments under the new system?
If you are enrolled in one of the new Medicaid Managed Care health plans, you will need to call your health plan to schedule a ride to and from your appointments. If you stayed in NC Medicaid Direct, you can still arrange transportation through your local DSS office. If you have problems with your transportation arrangements, you should report these issues to the NC Medicaid Ombudsman.
What if I have special health care needs?
Many people who were receiving services for severe behavioral health needs or intellectual/developmental disabilities before Medicaid transitioned to Managed Care were not required to enroll in a new Medicaid Managed Care health plan, and remained in NC Medicaid Direct. If you need services to address serious mental illness, serious emotional disturbance, severe substance use disorder, intellectual/developmental disability or traumatic brain injury, but you have been enrolled in a new Medicaid Managed Care health plan, you can reach out to the NC Medicaid Ombudsman to learn more about what your options are to ensure you get the services you need.
I have other questions about the new system, where can I go?
The NC Medicaid Ombudsman is a third party resource designed to help people through the transition to Medicaid Managed Care and to help them use their Medicaid coverage to get the services they need. The NC Medicaid Ombudsman can answer many questions and connect you to helpful resources. They can be reached toll-free at 877-201-3750, 8 a.m. to 5 p.m., Monday through Friday, except State holidays. Or you can visit them online at ncmedicaidombudsman.org.